Targeting chronic pain
Pain is an important protection system of the human body. But when it becomes chronic, as it frequently does, it no longer fulfils a meaningful function. Patients develop a so-called pain memory, making the pain an illness in its own right and disconnecting it from its original cause. Given the great number of sufferers and the complexity of the issue, the research community pays close attention to this phenomenon. Genetic and brain research seem to be well on the way towards understanding what causes chronic pain. Ruth Drdla-Schutting from the Medical University of Vienna is one of the researchers who are obtaining new answers to hitherto unresolved questions.
Analysing mechanisms
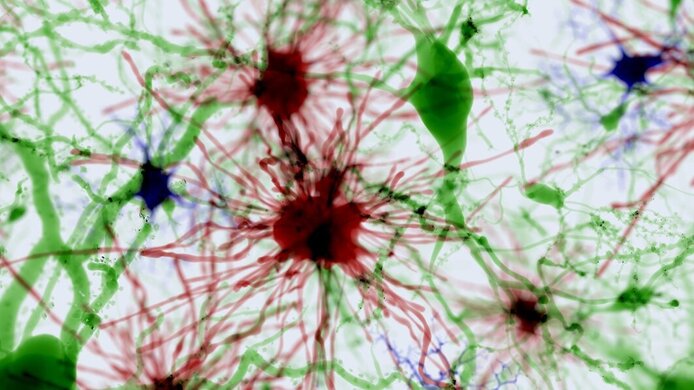
The neurophysiologist studies processes at cellular level in the central nervous system, which is where pain becomes manifest. In more concrete terms, Drdla-Schutting investigates the role of astrocytes, the most frequent type of cell in the central nervous system. A concrete mechanism triggering pain memory occurs at the point of contact of nerve cells in the spinal cord. This mechanism is called synaptic long-term potentiation (LTP). “For a long time, researchers concentrated only on nerve cells when investigating LTP”, explains Drdla-Schutting. “We know, however, that astrocytes also have a role to play in synaptic transmission”. Recently, researchers have been able to demonstrate that astrocytes play a role in LTP at the hippocampus – a region of the brain responsible for learning and memory. “To date, the results are subject to controversial discussions in the scientific community”, says Drdla-Schutting and points out that research in this field is still in its infancy. According to the scientist, there is even less certainty about what role astrocytes play in the spinal cord when it comes to the induction of pain. “This is mainly due to the fact that we lack the tools to selectively block or activate these cells.”
Targeting the root cause of pain
But the scientists are on the right track. – In animal experiments, they have been able to reverse some forms of chronic pain by administering high doses of “cell blockers”. Ruth Drdla-Schutting is now working on addressing astrocytes specifically, or, in other words, on blocking only this type of cell in cases of chronic pain, which she believes will produce better results with fewer side effects. In preparation for such targeted experiments, a Schrödinger Fellowship awarded by the FWF took the scientist to the Paris Descartes University, where she worked until recently on an innovative chemogenetic method in the team of the neuro-scientist Cendra Agulhon.
Bespoke methods
In Paris, Ruth Drdla-Schutting established a method for using astrocyte-specific DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) in the spinal cord. She does this by using genetically designed receptors which sit on the surface of cells where they act as sensors and transmit signals to the inside of the cell. These engineered receptors work like their natural counterparts, with the one difference that they can no longer be activated by substances the body produces itself. Instead, they are specifically activated by the administration of a certain compound (Clozapine-N-Oxide). DREADDs can be applied to various cell types, including astrocytes – which explains why they are of interest in this particular case. As a next step, Drdla-Schutting is now studying the impact on pain memory of activating astrocytes by means of DREADDs. Initial investigations are under way at the Center for Brain Research at the Medical University of Vienna.
Hoping for innovative therapies
Although DREADDs are currently employed only in basic research, researchers hold high hopes for this new technology, as the results of pre-clinical studies in cellular and animal experiments are very promising. Scholars hope to be able to use these receptors not only for chronic pain, but also for treating diseases such as epilepsy, Parkinson’s or diabetes.
Personal details Ruth Drdla-Schutting investigates the neuro-biological bases of chronic pain at the Center for Brain Research at the Medical University of Vienna. From 2014 to 2015 she did research at the renowned Paris Descartes University within the context of an Erwin Schrödinger Fellowship funded by the FWF.