The evidence suggests IL-6
As yet, there is no clear insight into which tumors trigger cachexia and how. “As a rule, tumors that send out signals for cachexia do not grow any faster. This means that they do not derive benefit from it, and it seems to happen by chance,” explains Schweiger. These are often small tumors from secretory tissues such as the pancreas. Prominent examples of people who experienced drastic weight loss as a result of their cancer disease are actor Patrick Swayze and Steve Jobs.
In the course of the research project, Schweiger's team made a crucial observation by chance: a cancer cell line that did not originally cause cachexia in mice had gone through normal mutation processes and ended up as a cell type that suddenly did cause pathological weight loss.
Serendipity
“That was a stroke of luck for us,” says Schweiger. “It allowed us to compare two cell lines that differ in their ability to trigger cachexia.” A comparison of these cell lines revealed signaling molecules that are produced uniquely by the cells that cause cachexia. These molecules included cytokine interleukin-6 (IL-6), a signaling substance of the immune system. In conjunction with a receptor in the blood, IL-6 forms a complex that docks onto various body cells and triggers the degradation of muscle tissue, for example. “After we removed IL-6 from the cancer cells and also from the bloodstream, the previously cachectic tumors no longer induced cachexia,” reports Schweiger.
The group published the results in the Journal of Cachexia, Sarcopenia and Muscle and made their cell model available to the scientific community. Schweiger intends to investigate the exact molecular processes responsible in more detail in follow-up projects – but the results are already game changers for therapeutic methods.
A glimmer of hope?
“As part of the project and in collaboration with a partner from China, we have identified R-ketorolac as a potential treatment option for cachexia,” says Schweiger. This is the R-enantiomer of S-ketorolac, i.e. its chemically mirrored variant. S-ketorolac is a painkiller that is normally used after surgery, but does not help against cachexia in this form.
In experiments, the drug increased the number of T lymphocytes and lowered IL-6 levels in the blood. The effect: weight loss slowed down and the survival rate of the test mice increased even under chemotherapy conditions, as Schweiger's team reported in a paper. Following the promising preclinical results, the drug is currently being tested in a first clinical trial at Cedars-Sinai Medical Center in Los Angeles in patients with advanced pancreatic cancer.
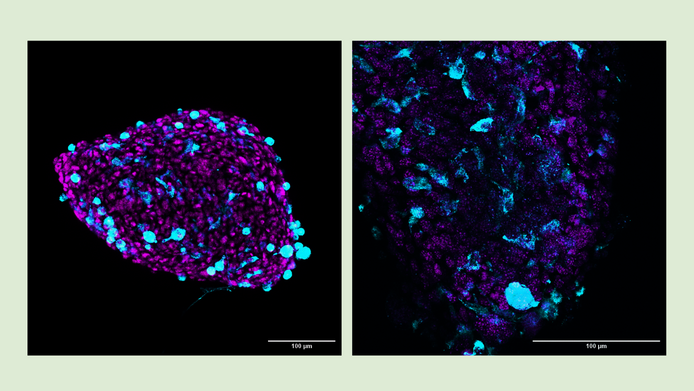
“The collaboration between clinicians and us, who do basic research, is essential,” emphasizes Schweiger. “We do the groundwork with cell cultures and mouse studies before large-scale clinical trials can be launched.”
Collaboration in Graz and Szeged
In order to better understand the metabolism of cachectic tumors, Schweiger's group is working closely with partners in Graz and Szeged (Hungary). Clemens Diwoky from the University of Graz used magnetic resonance spectroscopy to examine the tumors for their lipid content, energy status and blood flow. “He succeeded in developing a method to measure the energy status of a tumor in a living organism – in this case, in mice,“ notes Schweiger regarding the results of a third publication that emerged from the project.
Together with their Hungarian partners, the researchers also analyzed the lipid metabolism of cachectic and non-cachectic tumors. The results showed that lipid balance significantly influences tumor growth, whereas it does not affect cachexia. “Over the course of the project, we increasingly focused on IL-6 rather than lipids, as this was the more promising route,” notes Schweiger.