Why a myocardial infarction is often followed by a second one
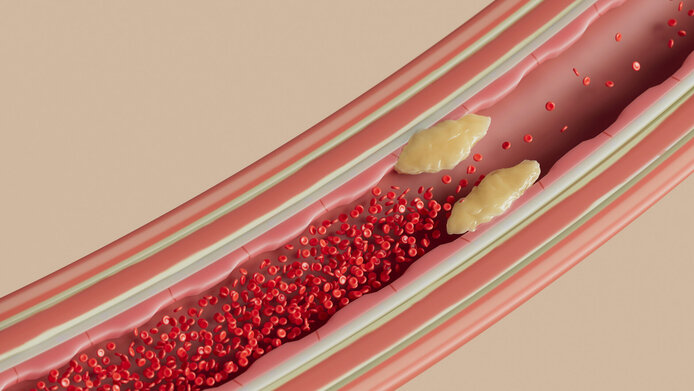
After the infarction is before the infarction: this is the sad truth for many patients. A myocardial infarction (MI) is usually triggered by atherosclerosis. This “calcification” of the blood vessels results in damage to the vessel wall and clot formation. These clots cut off the supply of blood and oxygen to the heart. The atherosclerotic plaques, i.e. the deposits on the artery walls, build up over decades – the unhealthier the lifestyle, the more severe plaque formation will be. Once an MI has occurred, however, it often takes just a few months or years for a second one to follow. The risk of further clot formation increases dramatically.
Excessive immune reaction
The culprit is an accelerated atherosclerosis, which in this case is no longer predominantly caused by classic risk factors. Researchers now understand that the process is linked to an immune reaction triggered by the infarction, which leads to a rapid increase in inflammatory processes in the blood vessels. Dimitrios Tsiantoulas and his team at the Medical University of Vienna have set out to decipher the exact mechanisms behind this phenomenon in order to prepare the ground for future therapies. Tsiantoulas' research group has joined forces with the teams of Amanda Foks from Leiden University and Julia Polansky-Biskup from Charité Universitätsmedizin Berlin in a project focusing on the B cells of the immune system.
“We have investigated how age and a previous MI influence the immune system's response. B cells are particularly good candidates in this context,” notes Tsiantoulas. “They are part of the adaptive immune response, which is trained through contact with pathogens or vaccines. B cells store this information for a long time and wait to rediscover an antigen known to them. The question is whether – and if so, why – their activation is also stepped up by plaques after an MI.” One of the hypotheses of molecular biologist Tsiantoulas posits a kind of mix-up that leads B cells, which actually ought to react to substances from dead heart muscle cells, to mistakenly intensify the inflammation on the plaques.
Survivors of a myocardial infarction have a particularly high risk of recurrent heart attacks. Studies show that this is due to an accelerated development of atherosclerosis (plaques). The B-eatATHERO project is investigating the role of the immune system, more specifically B lymphocytes, in the formation of plaques.
Systematic analysis of B cells
In the project, the Vienna-based research team aimed to find out which B cells actually react to an MI, given that these immune cells with a good memory for pathogens are anything but a homogeneous group. “The term B cell covers a whole family of cell types. That’s why we have used a mouse model for a systematic investigation of how all these groups behave after an infarction,” explainsTisantoulas.
At the same time, his colleagues in Leiden, the research team of Amanda Foks, carried out a similar study which tested the reaction of the various B cells to age-related atherosclerosis – i.e. in the absence of an MI. They also examined cells from human plaques, which are routinely extracted during operations, in order to establish a comparison with the mouse model. The Berlin team was in charge of the epigenetic investigations. “Julia Polansky-Biskup's team examined which permanent changes the genome of the immune cells underwent after an MI or after contact with age-related atherosclerosis,” explains Tsiantoulas.
The project’s outcomes actually took the researchers a big step closer to understanding the immunological processes following a myocardial infarction. Tsiantoulas and his colleagues were able to prove that the number of B cells actually increases significantly in this case, but that was not all. They apparently also have very specific properties. “The B cells develop a unique profile of gene expression – which regulates which type of genetic information is used to form proteins, for example. But this profile was never observed in animals with atherosclerosis that did not suffer an infarction,” explains Tsiantoulas.
Next research steps
Follow-up projects will now drill deeper into this discovery. “The next step is to find out what the consequences are of this unique genetic profile being formed. Which proteins are produced, and what information is inscribed in the memory of the B cells?” the researchers wonder. As soon as the signaling pathway and its connection to accelerated atherosclerosis have been revealed, researchers can start thinking about how to modulate the immune system's response when developing therapies.
“An antibody, a so-called small molecule, or another compound, could be a helpful active substance. This active substance should intervene in the signaling pathway and regulate it so as to prevent the excessive immune reaction and restore some balance,” notes Tsiantoulas. He is optimistic that a corresponding mechanism can be found. “B cells are a good target for active substances and are already being addressed in a whole range of other therapies.”
It may even be possible to adapt an already approved drug for this new application. Alternatively, mRNA technology – now also available in applications since the Covid vaccinations – could be used to introduce information into the B cells that reverses their harmful activation, posits the researcher. Even if the necessary clinical trials are lengthy, there is a good chance that MI patients will no longer have to worry about a threat to their lives recurring in a short space of time.
Personal details
Dimitrios Tsiantoulas is Assistant Professor of Cardiovascular Immunology and head of a research group at the Clinical Institute for Laboratory Medicine at the Medical University of Vienna. He completed his doctoral studies at the Medical University of Vienna and at the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences (ÖAW) before taking up a postdoctoral position at the University of Cambridge funded by the British Heart Foundation. Set to run between 2020 and 2024, the project “The role of B cell immunity in accelerated atherosclerosis” (B-eatATHERO) received EUR 300,000 in funding from the Austrian Science Fund FWF.
Publications
Smit V., de Mol J., Schaftenaar F.H., Depuydt M.A.C. et al.: Single-cell profiling reveals age-associated immunity in atherosclerosis, in: Cardiovascular Research 2023
Smeets D., Gisterå A., Malin S.G., Tsiantoulas D.: The Spectrum of B Cell Functions in Atherosclerotic Cardiovascular Disease, in: Frontiers in Cardiovascular Medicine 2022
Tsiantoulas D., Eslami M., Obermayer G. et al.: APRIL limits atherosclerosis by binding to heparan sulfate proteoglycans, in: Nature 2021





