Viruses as risk factors for coeliac disease

Digestive problems, severe inflammation of the small intestine and nutritional deficiencies leading to anaemia and osteoporosis force patients of the autoimmune condition coeliac disease to follow a strict gluten-free diet for life. In coeliac patients, gluten, a protein contained in many types of cereals, causes the immune system to attack the intestine. It has already been confirmed that the number of people being diagnosed with coeliac disease has increased significantly in recent decades and that those affected by the condition are at greater risk of developing other autoimmune diseases; however, less is known about the actual triggers of the disease. According to recent research, in addition to genetic factors certain viral diseases could be associated with its increased incidence. This indication prompted Reinhard Hinterleitner to take a closer look at this possible link and triggering process. A research laboratory specialized in coeliac disease at the University of Chicago provided the cell biologist with optimal conditions for his study, which he carried out as part of his FWF-funded Erwin Schrödinger Fellowship.
Suspicious viruses at the crime scene
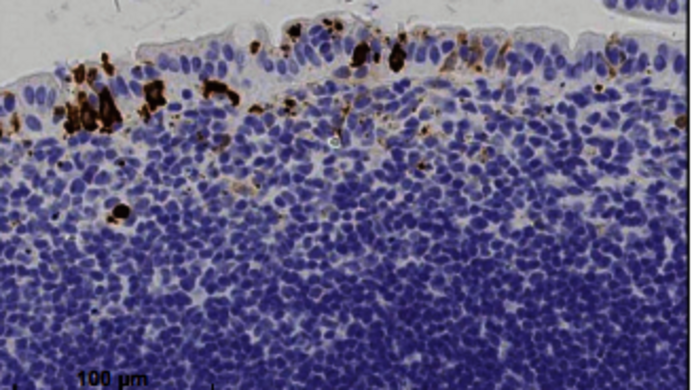
Hinterleitner's studies in the team of gastroenterologist Bana Jabri confirmed the strong link between intestinal viral infections and coeliac disease. He analysed samples of blood serum and 150 small-intestine biopsies from coeliac patients and compared them with those of a healthy control group: The focus was on intestinal viruses, for example the noro-, rota- and reoviruses. “Our analysis of the reovirus showed that coeliac patients had significantly more antibodies against this virus and these correlated with virus-associated markers in the biopsies. This means that it is highly probable that the coeliac patients had suffered from a recent or chronic intestinal viral infection," explains Hinterleitner.
Checkpoint small intestine
Another focus of the study was the question as to why coeliac patients lack oral tolerance to gluten: "Oral tolerance refers to the capacity of specialised cells in the small intestine known as dendritic cells to only activate an immune response in the presence of harmful invaders. To do this, the dendritic cells present gluten antigens to the T cells; these do not usually trigger an inflammatory response in the presence of gluten antigens. However, the dendritic cells of coeliac patients always sound the alarm bells in the presence of gluten proteins. Incorrect information is transmitted to the T cells or T lymphocytes, to be precise, and they react to this information with a pro-inflammatory response," says Hinterleitner.
Viruses trigger false alarm
Viruses can become the trigger of the long-term false alarm in coeliac patients: "Intestinal viruses upset the small intestine and regulatory T lymphocytes can be transformed into pro-inflammatory T lymphocytes as a result," according to Hinterleitner. "The dendritic cells are also alerted by the infection. If gluten containing food is consumed at the same time as a viral infection occurs, the already alerted dendritic cells also present gluten antigens to the T lymphocytes." This can result in the transmission of incorrect information and the T lymphocytes react with an inflammatory response, which is aimed not only at the virus but also at the gluten.
Man & mouse
Hinterleitner observed this process in a genetically engineered coeliac mouse model: "In the case of a reoviral infection of the small intestine of mice, similar clinical symptoms to those experienced by coeliac patients arose when gluten was consumed at the same time." This inauspicious timing could result in a long-term loss of oral tolerance to gluten in the 20 percent of the population with the genetic predisposition for coeliac disease, and particularly in patients who respond more strongly to virus infections.
Children as a risk group
This could also explain why infants who have already had a rotavirus infection are more likely to develop coeliac disease: "The first intake of gluten by infants, which is supposed to establish oral tolerance to gluten, can have precisely the opposite effect if the child is suffering from a viral infection at the same time," explains Hinterleitner. Thus, vaccination against intestinal viruses such as rota- and reovirus in early childhood could reduce the incidence of coeliac disease in risk groups. This FWF project not only presents insights into the emergence of coeliac disease and possible approaches for halting its further spread, it also explains the possible processes underlying the emergence of other autoimmune diseases such as type 1 diabetes and rheumatoid arthritis.
Personal details Reinhard Hinterleitner studied molecular biotechnology at the FHWien University of Applied Sciences. He received his PhD from the Medical University of Innsbruck in molecular cell biology and oncology at the group of Gottfried Baier at the Department of Medical Genetics, Molecular and Clinical Pharmacology. He is currently carrying out his postdoctoral research at the University of Chicago in the group of gastroenterologist Bana Jabri at the Department of Medicine & Committee on Immunology. His research residency there started in the course of an Erwin Schrödinger Fellowship conferred on him by the FWF.