Reading tip
The book "Besser schlafen" (in German) by Birgit Högl provides the latest findings in neuroscience; Brandstätter-Verlag 2023

People who suffer from a sleep disorder are not themselves while they are asleep or dreaming. “For instance, they will be aggressive or dangerous. Anyone sharing their bed may end up with a busted lip or a black eye. And they are also prone to hurting themselves, for instance when they fall out of bed,” says Birgit Högl, a neurologist and head of the Sleep Disorders Unit at the Medical University of Innsbruck. These nocturnal outbursts are usually caused by a condition called Isolated REM Sleep Behavior Disorder (iRBD). REM, or rapid eye movement, denotes the sleep stage during which a healthy person usually does not move at all. Högl estimates that one in 100 people suffers from iRBD, which affects men and women equally and is more frequently diagnosed in older people. That being said, exact numbers are hard to come by as those afflicted are often not aware of their condition, and patients who present with the corresponding symptoms usually need to wait for a long time to be examined.
Against this backdrop, Högl’s research group has developed a unique tool. In collaboration with Heinrich Garn and Bernhard Kohn of the Austrian Institute of Technology (AIT), Högl and her team equipped a high-tech camera with artificial intelligence capabilities to detect iRBD-specific movements. “The method has turned out to be so exact that it is fit for use in the hospital,” says Matteo Cesari, a bioengineer and the lead author of a current study that is part of the project. The Austrian Science Fund (FWF) financed the project, which has by now turned into an EU project in which researchers are further developing the technology to make it suitable for mass screenings. iRBD presents a risk not only to the people affected and those sleeping close to them, it is also the most sensitive and specific marker for dying nerve cells. To slow down this neurodegenerative process, it is key to diagnose it as early as possible.
A sleep disorder is easy to detect when the person concerned has trouble sleeping. For disorders such as iRBD, a diagnosis is much more difficult to come by. If a person suffers from iRBD, their muscles are not paralyzed during the REM stage the way they are in healthy people. “The legs and arms of iRBD patients tend to twitch rapidly. They also move in a way that looks like they are acting out their dreams lying down,” Högl describes the symptoms.
The sleep expert thinks that it is due to social reasons that iRBD is more often diagnosed in men: while many women are single and sleep alone at later stages of their life, older men share their bed more often, so that the disorder is more easily found. In general, however, it often goes undetected. “Some people don’t even know that it is not normal to actually carry out all the movements you are dreaming about in your sleep,” Högl says.
A person older than 50 who suddenly starts to move or behave strangely (with or without dreams) during their sleep is well advised to consult a sleep lab. For one thing, physicians can prescribe medication that can ease the symptoms of iRBD. For another, the disorder is a clear indication of the loss of nerve cells and is thus often associated with other diseases. “Ninety percent of all patients with iRBD develop a neurodegenerative disease such as Parkinson’s, Lewy body dementia or multiple system atrophy (MSA),” Högl says. Often, this happens over the course of several years.
This is why iRBD patients are an ideal target group for newly developed drugs that can help slow down the degenerative process. At the moment, a lot of research is carried out in this field, among others by Ambra Stefani and her colleagues from Högl’s unit. They know that if patients suffer from one of the above-mentioned diseases, many of their nerve cells have already died. “An iRBD diagnosis can give us a ten-year head start. But the sleep lab is currently the needle’s ear,” the neurologist points to the weak link in the system.
For the moment, sleep disorders can only be reliably diagnosed in sleep labs. In a polysomnography, various signals are monitored in a sleeping person, among other things brain activity (EEG), eye movements, breathing patterns, noise, muscle tone and body posture. The data are collected and manually assigned to the various sleep stages. As this requires a lot of staff and time, patients have to wait for a year or longer to get an appointment in a sleep lab in Austria. Högl’s research group has addressed this shortcoming by creating an automated solution for diagnosing iRBD. Their goal was to come up with a tool that could also be used to screen healthy people in order to detect the risk of developing a neurodegenerative disease early on.
Birgit Högl has headed the Medical University of Innsbruck’s sleep lab for 24 years. She specializes in sleep disorders and was appointed Professor for Neurology with a focus on Sleep Medicine in 2019.
Matteo Cesari studied Bioengineering in Italy and Denmark. He joined Birgit Högl’s research group as a post-doctoral researcher four years ago.
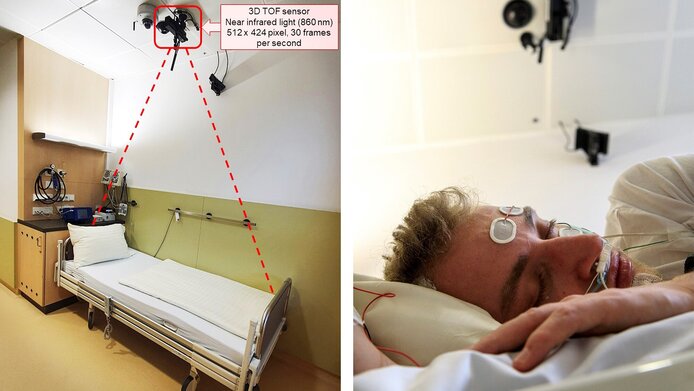
“The time-of-flight camera we use for our method is also used as a Kinect sensor in the Xbox console,” Cesari explains the construction. The 3D camera emits infra-red radiation, which is reflected by the sleeping person’s body. By measuring the reflected signals, the distance between the camera and the person can be calculated. “We take 30 pictures a second and get the distance for every pixel. If the distance changes, we know that the person has moved in their sleep,” the bioengineer explains.
To analyze the camera data, the researchers developed an AI-based solution to minimize manual steps as far as possible. In their study, Cesari and his colleagues presented the newest version of the system, which merges analysis data of several body parts using a machine learning mechanism. “We collate the movements of the person’s legs, torso, hands and head during REM sleep. Superimposing the data onto each other this way gets us the best results,” Cesari explains. The system’s detection rate for iRBD patients is 87%, which is close to the – much more resource-intensive – multi-factor examination in the sleep lab. As a next step, the system will be fine-tuned with the help of an EU-wide cooperation.
To diagnose iRBD, the system needs to identify the movement data from the REM stage. For now, this step still requires additional measurements. “We are currently working on turning it into a stand-alone method. To this end, we are coordinating a study with 300 test subjects,” Cesari shares more details about the project, in which sleep labs from Germany, Italy, Spain and France will participate. The team is also trying to downscale the hardware from currently 2 kilograms to 13 grams to turn it into a mobile device.
The team’s vision is to develop what they describe as “an automated sleep lab fit for home use”, which could be used for comprehensive screenings across the population. People who belong to risk groups could particularly benefit from this system. This includes, e.g., occupants of retirement homes for whom the trip to the hospital may be difficult. “A person developing iRBD requires a solid diagnosis, consultation and check-ups,” Högl firmly states. “They should understand their condition and know that it is possible to delay the progress of a neurodegenerative disease.”
The project “Advanced Video and Audio Analysis of Sleep Disorders with Motor Manifestations” was carried out in cooperation with the Austrian Institute of Technology (AIT) and received funding by the Austrian Science Fund (FWF) in the amount of EUR 315,642. The results have laid the groundwork for the EU project “BRAVA – Behaviours in REM sleep: personalised Automatic 3D Video Analysis as novel tool to detect alpha-synucleinopathies”, which is currently under way.
The book "Besser schlafen" (in German) by Birgit Högl provides the latest findings in neuroscience; Brandstätter-Verlag 2023
![[Translate to English:] Buchcover Besser Schlafen](/fileadmin/_processed_/8/e/csm_Warum_guter_Schlaf_so_wichtig_ist_ef88fe16e0.png)